America's Public Health Amnesia is Bringing Measles Back
America's collective amnesia about preventable diseases isn't failure—it's a political choice with a body count.
In West Texas, a school-age child died of measles last week—the first death in an outbreak now spanning two states. The child was unvaccinated. Their death wasn't inevitable or mysterious. It resulted from a preventable disease America conquered decades ago. As officials gathered for a somber press conference at Lubbock's Covenant Medical Center, the tragedy laid bare a collective failure and an uncomfortable truth: America suffers from public health amnesia.
Before vaccination became widespread, measles infected an estimated 3-4 million Americans annually. Each year, it hospitalized 48,000 people, caused encephalitis in 1,000, and killed between 400-500 individuals—primarily children. Beyond those immediate numbers were countless connected cases of pneumonia, permanent hearing loss, and intellectual disabilities. For every 1,000 children infected, one or two died. A 2015 study suggested that measles may have accounted for half of all infectious disease deaths in children before vaccination.
The 1963 introduction of the measles vaccine was one of medicine's greatest triumphs. By 2000, the disease was declared eliminated from the United States—meaning no continuous transmission occurred within American borders for 12 months. This victory wasn't some happy accident. It took sustained, coordinated public health campaigns, school vaccination requirements, and robust disease monitoring.
But public health victories aren't permanent unless the society that benefits from them chooses to maintain them. Polio— the terror of your grandparents' summer - has now been almost forgotten thanks to vaccination. But declining immunization rates are threatening this achievement too. Other examples: Tuberculosis resurged in the 1980s and 1990s after funding cuts to control programs. Clean water systems, food safety protocols, and anti-smoking campaigns follow the same patterns—once successful, they become invisible and vulnerable to budget cuts, deregulation, and crankery.
It's a cycle, and it's painfully predictable. First comes crisis and mobilization. Next, success and celebration. Then complacency as memories fade. Finally, regression through funding cuts, politicization, and infrastructure decay. And when the threat inevitably returns, the public is shocked, as if the outcome couldn't have been foreseen. The institutional memory that would connect cause and effect has been dismantled.
Since late January, Texas health officials have identified 124 measles cases, primarily among unvaccinated children and teenagers. Eighteen have required hospitalization. The outbreak began in Gaines County, Texas, home to thousands of Mennonites—an insular Christian community with historically lower vaccination rates—before spreading to neighboring counties and across state lines. New Mexico has reported nine additional cases in Lea County, which borders Texas, including four unvaccinated children.
These outbreaks correlate directly with vaccination gaps. Gaines County's measles vaccination rate is approximately 82%, significantly below the 95% threshold that experts identify as necessary for herd immunity. This pattern extends nationally. According to CDC data, the kindergarten measles-mumps-rubella (MMR) vaccination rate for the 2023-24 school year sits just under 93%—a figure that hasn't rebounded from pandemic-era declines. These averages hide deadly vulnerabilities in specific communities where rates fall far lower, creating pockets of susceptibility where measles, which can infect up to 18 others from a single case, spread explosively.
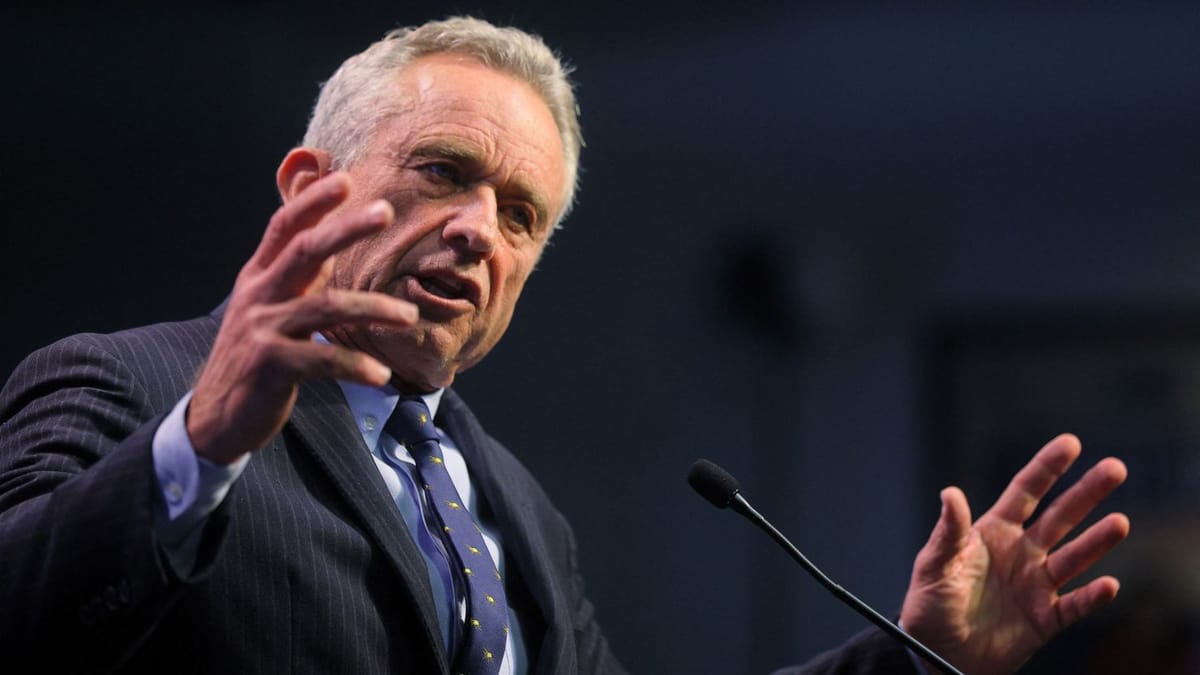
The appointment of Robert F. Kennedy Jr. as health secretary is an unprecedented elevation of disproved, debunked, irresponsible, eugenics-driven vaccine skepticism to the highest levels of public health leadership. At a White House cabinet meeting responding to the child's death, Kennedy downplayed the outbreak as "not unusual," offering no mention of vaccination as a preventive measure. His published statements that "measles outbreaks have been fabricated to create fear" and that vaccines exist "for the sole purpose of fattening industry profits" now carry the weight of official authority, undermining confidence in proven life-saving interventions.
Vulnerable communities exist throughout America. Religious groups like the Mennonites in Texas, isolated rural populations, and neighborhoods with limited healthcare access are all opportunities for measles to gain footholds. When vaccination rates drop even slightly in these communities, the mathematical certainty of outbreaks follows.
Overlapping systemic failures have manufactured America's public health amnesia. Social media algorithms amplify sensational claims and utterly bury actual, fact-based explanations. Anti-vaccine content spreads six times faster online than factual information. Digital platforms create echo chambers where parents encounter false controversy instead of medical consensus, turning vaccination from a medical necessity, which has always been a perceived matter of personal taste.
The generational gap compounds this problem. Americans born after widespread vaccination implementation have no direct experience with diseases like measles. The parents currently declining vaccines never witnessed classmates develop encephalitis or siblings struggle for breath with diphtheria. Without reference points, many cannot recognize the abnormality. Abstract statistics prove poor competitors against vivid - entirely fabricated - anecdotes about alleged vaccine injuries.
Meanwhile, America has been dismantling its own public health infrastructure for decades. Local health departments lost over 20% of their workforce between 2008-2019. The pandemic briefly reversed this trend, but emergency funding has dried up. Monitoring systems, community outreach programs, and immunization campaigns operate on skeleton budgets—until crisis strikes.
The final component is political polarization. Public health measures, from vaccination to masking, have become tribal identifiers. Politicians cynically see electoral advantage in opposing public health protocols rather than supporting them. This polarization cuts across institutional lines, turning health departments into political battlegrounds where science competes with ideology, eroding professional authority and public trust.
Without intervention, the United States will face potential disease outbreaks that were long considered historical footnotes. And each one will lead to preventable suffering, unnecessary death, and massive healthcare costs.
A 2019 measles outbreak in Washington state cost public health agencies $3.4 million to contain—twenty times what prevention through vaccination would have cost. Multiply this across states and diseases, and the irresponsibility is staggering.
If the United States struggles to maintain immunity against known pathogens with proven vaccines, how will it respond to novel viruses or antibiotic-resistant bacteria? It's a downward spiral that threatens to leave America vulnerable precisely when global health threats multiply.
Other countries - led by responsible leaders, rather than hyper-capitalist death cults and felonious memecoin salesmen - maintain higher vaccination rates through institutional memory preservation. Japan and Taiwan's public health museums document disease impacts, while Australia's "No Jab, No Pay" policy links childhood benefits to immunization status, creating consistent incentives regardless of political shifts.
But insulating public health from political volatility means governance reforms. Independent public health agencies with dedicated funding streams—modeled after the Federal Reserve's independence—are the only way to maintain disease prevention continuity across administrations. Vaccination policies have to become bipartisan infrastructure, not partisan battlegrounds.
Media organizations have to recognize their responsibility in public health reporting. False equivalence between scientific consensus and fringe views creates controversy where none exists. Journalism that contextualizes disease risks and prevention benefits—rather than sensationalizing rare adverse events in pursuit of clicks—serves the public interest.
If those shifts seem unlikely in the near term, community-based approaches show more promise. When trusted local leaders—religious figures, teachers, and community organizers—advocate for vaccination, rates increase significantly.
But without any of those changes, the outlook is grim.
America can keep on dismantling public health infrastructure until preventable diseases become commonplace again, or it can reclaim the hard-won knowledge previous generations secured at tremendous cost. But that choice - between learning from history and repeating - it has real consequences, measured in lives lost.
As Robert F. Kennedy JR flips bullish on Measles, Americans must ask themselves what other vanquished threats await resurrection through neglect. Polio? Diphtheria? Smallpox? Each represents a victory that can be very easily undone. Public health advances are reversible—and reversing them extracts payment in human suffering. The bill for forgetting always comes due.
Now, more than ever, the world needs an independent press that is unencumbered by commercial conflicts and undue influence.
By taking out an optional founding membership, you can help us build a free, accessible, independent news platform firewalled from corporate interests.
Support The Index


